Llantrisant
Sub-Aqua Club
www.llantrisantdivers.com
|
|
|
|
|
|
|
|
| |
|
Travel
Health Information
|
|
|
 Since the number of divers
travelling abroad in search of new and exotic locations in
which to dive is on the increase, there is a growing need
for information about health protection in these foreign countries. Since the number of divers
travelling abroad in search of new and exotic locations in
which to dive is on the increase, there is a growing need
for information about health protection in these foreign countries.
We all look forward
to our trips abroad but the experience can be spoiled if we
become unwell whilst away.
 However,
most (but not all) of the world's
exotic dive locations are located in and around the
tropics and are accessed via developing countries,
where there are endemic health
issues and the
standard of healthcare is often below that of the UK. However,
most (but not all) of the world's
exotic dive locations are located in and around the
tropics and are accessed via developing countries,
where there are endemic health
issues and the
standard of healthcare is often below that of the UK.
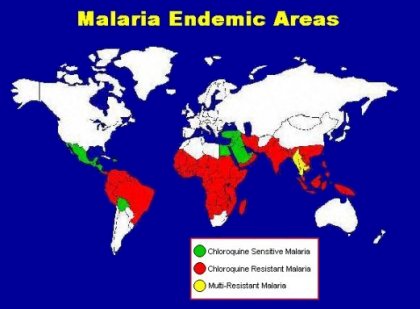
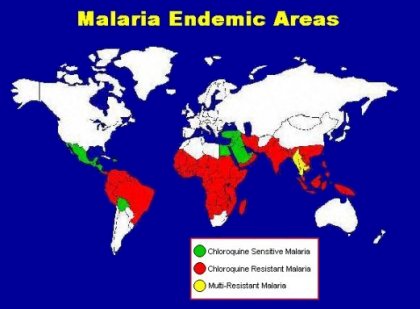
There is therefore a risk of
contracting a more serious illness like malaria, yellow fever,
typhoid, hepatitis, etc. so it
is vital that travellers take certain precautions before,
during and after travel. It may also
be necessary to be protected against certain diseases by vaccinations
prior to travel or by taking tablets during and after the
trip.
 The table below
contains information about vaccination requirements and malaria
prophylaxis for travellers going abroad and contains most
of the countries likely to be visited by divers going on diving
holidays and expeditions. The table below
contains information about vaccination requirements and malaria
prophylaxis for travellers going abroad and contains most
of the countries likely to be visited by divers going on diving
holidays and expeditions.
 In addition to malaria
tablets and the various vaccinations required, persons travelling
to developing countries are strongly advised to carry a medical
kit containing a number of medical and first aid item. In addition to malaria
tablets and the various vaccinations required, persons travelling
to developing countries are strongly advised to carry a medical
kit containing a number of medical and first aid item.
Most reputable dive operations will carry a first aid
kit and basic medical items in addition to oxygen for diving
accidents at the dive centre or aboard their charter boats.
It may be worth checking with the tour operator before travelling.
For
examples of
basic medical and
first aid kits:- |
|
|
|
|
Fortunately,
most minor complaints associated with travel such as holiday
tummy, diarrhoea, travel sickness, sunburn, insect bites,
etc. can easily be treated by carrying the appropriate remedies
in a basic medical kit and a first aid kit:-
|
|
|
|
|
|
Table
of Malaria Prophylaxis
and Vaccinations for Travellers |
| |
|
 The
list of countries in the table below is by no means exhaustive
and should only be used for quick reference purposes. The
data in the table only applies to healthy adults. Travellers
will need to consult their own doctor to arrange to have the
relevant vaccinations. The
list of countries in the table below is by no means exhaustive
and should only be used for quick reference purposes. The
data in the table only applies to healthy adults. Travellers
will need to consult their own doctor to arrange to have the
relevant vaccinations.
The advice
in the table is for travellers visiting
a single country and arriving directly from the UK. It is
intended for use by persons planning a short stay i.e. less
than three months.
Specialist advice
should be sought by persons intending to live abroad for
long periods or for persons travelling between countries.
For long stays (over three months) and for trips to remote
areas, vaccines not mentioned below such as Rabies, Diphtheria
or Hepatitis B may be required.
The information
is not designed for use by pregnant women, nursing mothers,
children or persons suffering from epilepsy or any other chronic
condition who should consult their doctor before taking malaria
tablets.
No particular
immunisation or malaria prophylaxis is required for direct
travel to Europe, U.S.A., Canada, Australia or New Zealand.
However travellers should be advised to make sure that they
have had a tetanus booster within the previous ten years.
|
Country
|
Malaria
Tablets
|
Typ
|
Tet
|
Pol
|
Hep
A
|
Yel
|
Men
|
|
Mediterranean
|
|
Cyprus
|
NONE
|
---
|
R
|
---
|
R
|
---
|
---
|
|
Malta
|
NONE
|
---
|
R
|
---
|
R
|
---
|
---
|
|
Turkey
|
C
|
R
|
R
|
R
|
R
|
---
|
---
|
|
|
|
|
|
|
|
|
|
|
Africa
|
|
Egypt
(Red Sea)
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Kenya
|
A
|
R
|
R
|
R
|
R
|
R
|
R
|
|
South
Africa
|
A
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Tanzania
|
A
|
R
|
R
|
R
|
R
|
M
|
R
|
|
Zanzibar
|
A
|
R
|
R
|
R
|
R
|
M
|
R
|
|
|
|
|
|
|
|
|
|
|
Asia-Pacific
|
|
Australia
|
NONE
|
---
|
---
|
---
|
---
|
---
|
---
|
|
Bali
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Indonesia
|
A
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Malaysia
|
A
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Maldives
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Myanmar
|
A
|
R
|
R
|
R
|
R
|
---
|
R
|
|
Papua
New Guinea
|
A
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Philippines
|
B
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Phuket
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Singapore
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Thailand
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
|
|
|
|
|
|
|
|
|
The
Americas
|
|
Bahamas
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Cayman
Islands
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Costa
Rica
|
C
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Cuba
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Dominican
Republic
|
C
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Ecuador
|
A
|
R
|
R
|
R
|
R
|
R
|
---
|
|
Galapagos
Islands
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Jamaica
|
NONE
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Mexico
|
C
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Leeward
Islands
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
Windward
Islands
|
D
|
R
|
R
|
R
|
R
|
---
|
---
|
|
U.S.A.
|
NONE
|
---
|
---
|
---
|
---
|
---
|
---
|
| |
|
R = Recommended |
|
M = Mandatory |
| Typ
= Typhoid |
|
Tet = Tetanus |
| Pol
= Polio |
| Hep
A = Hepatitis A |
| Yel
= Yellow Fever |
| Men
= Meningitis |
|
Please
Note:
The above table is for
quick reference only.
For more comprehensive information go to the
Travel
Doctor web site. |
|
| |
|
|
| Malaria
Prophylaxis |
|
Malaria tablets should be started
one week before entering the malarious zone, taken throughout
the duration of the stay and continuing for at least four
weeks after return without fail. All tablets should be taken
with or after food, preferably with the main meal of the day.
|
Regimen A -
|
Mefloquine one 250mg tablet
weekly. OR
Doxycycline one 100mg capsule daily. OR
Malarone one tablet daily.
|
|
Regimen B -
|
Chloroquine 300mg
weekly (2x150mg tablets). PLUS
Proguanil 200mg daily (2x100mg tablets).
|
|
Regimen C -
|
Chloroquine 300mg
weekly (2x150mg tablets) OR
Proguanil 200mg daily (2x100mg tablets).
|
|
Regimen D -
|
No
prophylactic tablets required but anti mosquito
measures such as insect repellents, mosquito nets, long
sleeved clothing, etc. should be strictly observed.
|
|
Proguanil = Paludrine Tablets;
Chloroquine = Nivaquine or Avloclor Tablets;
Mefloquine = Lariam Tables.
|
Patients with a history of psychiatric disturbances
(including depression) should not take mefloquine as it may
precipitate these conditions. It is now advised that mefloquine
be started two and a half weeks before travel. No other tablets
are required with mefloquine or doxycycline. Mefloquine can
be taken for periods up to one year, doxycycline should not
be taken for periods longer than three months. Doxycycline
does carry some risk of photosensitisation.
Please
Note:
No prophylactic regimen
is 100%
effective.
Some
forms of malaria can develop seven days after being bitten
by an infected mosquito and others can incubate for even longer.
Typical symptoms of malaria are bouts of high fever lasting
several hours starting dramatically with shaking chills, subsiding
with profuse sweating, and reappearing at regular intervals,
most commonly every 48 hours. Anybody experiencing any of
these symptoms (which could be confused with flu) within twelve
months of returning from a malarious zone should seek medical
advice immediately. Deaths have occurred in cases where where
the symptoms have been ignored until it is too late!
Since
protection against the malaria parasites may not be complete
it is important that measures are taken to avoid getting bitten
by mosquitoes:-
- Sleep
in screened rooms, using a fly killer spray to kill any
mosquitoes that may have entered the room during the day.
- Use mosquito
nets around the bed at night. Check that there are no holes.
Tuck the net under the mattress.
- Wear
long sleeved clothing and long trousers when outdoors after
sunset. Light colours are less attractive to mosquitoes.
- Use repellents
such as diethyl toluamide (DEET) on exposed skin or wear
DEET impregnated wrist bands and anklets.
- Clothing
and mosquito nets can be impregnated with a solution of
30ml DEET in 250ml water.
|
Remember:
Malaria can be fatal!
Worldwide,
two million people
die
from Malaria every year.
| The ABCD of Malaria Treatment |
|
 A: be Aware of the risk of malaria if you
are travelling to a foreign country. A: be Aware of the risk of malaria if you
are travelling to a foreign country.
 B: avoid mosquito Bites by taking appropriate measures.
Reducing the number of Bites reduces the chances of
getting malaria. B: avoid mosquito Bites by taking appropriate measures.
Reducing the number of Bites reduces the chances of
getting malaria.
 C: Comply
with the appropriate prophylactic drug regimen for
the area you are visiting. This is vitally important
since failure to comply places you at great risk.
Studies have shown that there is a reduced risk of
contracting malaria even if you take the wrong regimen. C: Comply
with the appropriate prophylactic drug regimen for
the area you are visiting. This is vitally important
since failure to comply places you at great risk.
Studies have shown that there is a reduced risk of
contracting malaria even if you take the wrong regimen.
 D: early Diagnosis of malaria if symptoms
manifest following travel to a malarious region is
vital. Malaria can be fatal but early diagnosis and
treatment is usually 100% effective. D: early Diagnosis of malaria if symptoms
manifest following travel to a malarious region is
vital. Malaria can be fatal but early diagnosis and
treatment is usually 100% effective.
|
|
|
|
What
is Malaria?
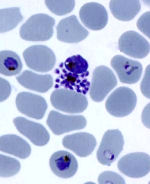
 Malaria is a disease
which you can catch by being bitten by a mosquito carrying
the malaria parasites in its saliva. The
species of mosquito that carries the malaria parasites is
the Anopheles mosquito. Malaria is a disease
which you can catch by being bitten by a mosquito carrying
the malaria parasites in its saliva. The
species of mosquito that carries the malaria parasites is
the Anopheles mosquito.
These
parasites then enter your bloodstream and travel to your
liver where they multiply and are released back into the bloodstream
in large numbers which then invade red blood cells.
They
continue to multiply until the red cells burst releasing
large numbers into the blood plasma causing the characteristic
fever associated with the disease. This phase of the disease
occurs in cycles of approximately 48 hours.
 The
free parasites are then able to infect any mosquito that
feeds on your blood during this phase. The cycle then continues
as the parasites multiply inside the mosquito and invade its
salivary glands. The
free parasites are then able to infect any mosquito that
feeds on your blood during this phase. The cycle then continues
as the parasites multiply inside the mosquito and invade its
salivary glands.
The malaria parasite is a microscopic organism called
a Plasmodium and it belongs to the group of tiny organisms
known as protozoans.
There are four types of plasmodium: P. falciparum (the
most dangerous), P. vivax, P. ovale & P. malariae.
Anybody travelling to an area where this mosquito is endemic
is at risk of catching the disease. Lately there has been
an increase in the cases of malaria reported in the UK - in
1993 there were 1922 reported cases in the UK, including five
deaths. All caught the disease abroad and almost all cases
could have been prevented.
|
|
| Vaccine
Information |
|
|
|
 Typhoid Typhoid
The original
typhoid vaccine was given in two doses at intervals of four
to six weeks and gave immunity for up to three years. 0.5ml
was given by subcutaneous or intramuscular injection or 0.1ml
by intradermal injection. This vaccine induced a mild form
of the illness which could be very unpleasant in certain cases.
Typhim
Vi is a single dose vaccine where 0.5ml is given by deep
subcutaneous or intramuscular injection. Immunity lasts for
approximately three years.
Vivotif
is a live oral vaccine contained in an enteric coated capsule.
The vaccine is taken as three doses of one capsule on alternate
days. The capsules should be stored in a refrigerator between
doses. Protection begins seven to ten days after the last
dose.
|
|
 Tetanus Tetanus
The Department
of Health recommends administration of reinforcing doses after
ten years, with the administration of further doses in the
event of injuries that may give rise to tetanus. 0.5ml is
given by deep subcutaneous or intramuscular injection.
|
|
 Polio Polio
Poliomyelitis
vaccine is recommended for long term travellers to areas which
have a high incidence of the disease such as developing countries.
Live oral vaccine is generally used. Three drops of the vaccine
constitutes a single dose. Initially three doses are given
at intervals of at least four weeks. Those who have been fully
immunised in the past will only need a single booster dose
every ten years if they intend to travel.
|
|
 Hepatitis
A Hepatitis
A
Hepatitis
A is associated with poor hygiene and sanitation. Havrix Monodose
is an inactivated vaccine prepared from the hepatitis A virus.
A single 1ml dose is given intramuscularly to give immunity
up to one year. To obtain immunity up to ten years a second
booster dose is given between six and twelve months of the
original.
Human Normal
Immunoglobulin (HNIG) contains antibodies to Hepatitis A and
will give protection for up to three months. 2ml of vaccine
is administered by deep intramuscular injection.
|
|
 Yellow
Fever Yellow
Fever
This is
given as a live vaccine (0.5ml subcutaneously) at designated
yellow fever centres where an international certificate of
vaccination will be issued and is valid for ten years, from
ten days after vaccination. The certificate may be required
for entry into certain countries particularly in East Africa.
It is recommended that the traveller carries the certificate
along with his or her passport when travelling to countries
at risk.
|
|
 Meningitis
(A&C) Meningitis
(A&C)
Meningitis
vaccine is recommended for travellers to areas where the disease
is endemic such as most of Sub-Saharan Africa. Saudi Arabia
requires vaccination of pilgrims to Mecca during the Hajj.
0.5ml of inactivated vaccine is given by deep subcutaneous
or intramuscular injection. Immunity lasts up to three years.
|
|
 Japanese
B encephalitis Japanese
B encephalitis
This is
a rare but serious insect borne disease that occurs in most
of the Far East and South East Asia. Vaccination is recommended
for stays of longer than one month in rural areas during and
just after the rainy season. The vaccine is issued on a named
patient basis and is given as 1ml subcutaneously for immunity
up to four years.
|
|
VACCINATION
SCHEDULES
|
- Inactivated
vaccines usually require one primary dose followed by one
or more booster doses given at intervals of around four
weeks. If time is short, a single dose will give some protection.
Most inactivated vaccines can be given together safely;
inactivated and live vaccines can also be administered simultaneously.
- When
two live vaccines are required, they should be given either
simultaneously at different sites or with a gap of at least
three weeks. Oral polio vaccine should not be given at the
same time as oral typhoid vaccine.
- Human
Normal Immunoglobulin (HNIG) may interfere with the immune
response to live vaccines and so should not be administered
simultaneously. A live vaccine should ideally be given three
weeks before or three months after an injection of HNIG.
However, HNIG is unlikely to contain antibodies to the yellow
fever virus and so they can be administered simultaneously.
Oral polio vaccine when given as a booster can also be administered
simultaneously with HNIG.
|
|
| Travellers
Diarrhoea |
| |
|
 Travellers'
diarrhoea (TD) is a condition characterised by a marked increase
in the frequency of unformed bowel movements and is commonly
accompanied by abdominal cramps, urgency, nausea, bloating,
vomiting, fever, and malaise. Travellers'
diarrhoea (TD) is a condition characterised by a marked increase
in the frequency of unformed bowel movements and is commonly
accompanied by abdominal cramps, urgency, nausea, bloating,
vomiting, fever, and malaise.
It
occurs in up to a half of European travellers who spend two
or more weeks in developing parts of the world and should
therefore be taken seriously.
Episodes
of TD usually begin abruptly, occur during travel or soon
after returning home, and are generally self-limiting. The
onset of TD is usually within the first week of travel, but
can occur at any time during the visit and even after returning
home.
The
most important determinant factor is the destination of the
traveller. High-risk destinations include most of Latin America,
Africa, the Middle East, and Asia, where attack rates of up
to 50% have been reported.
 TD
is slightly more common in young adults than in older people
but attack rates are similar in men and women. It is possible
for travellers to experience more than one episode of TD during
a single trip but rarely is it life threatening. TD
is slightly more common in young adults than in older people
but attack rates are similar in men and women. It is possible
for travellers to experience more than one episode of TD during
a single trip but rarely is it life threatening.
TD
is usually acquired by ingestion of faecally contaminated
food or water, or both. Both cooked and uncooked foods may
be implicated if they have been improperly handled. The place
in which food is prepared appears to be an important variable,
with private homes, hotels, restaurants, and street vendors
are listed in order of increasing risk.
Particularly
risky foods include raw or undercooked meat, poultry, seafood,
raw fruits and vegetables. Tap water, ice, and unpasteurized
milk and dairy products are also associated with increased
risk of TD. In the UK, we drink water straight from the tap
and rarely consider that the water may be the source of disease
but when the cleanliness of a water supply is in doubt, only
adequately purified water should be drunk.
 Worldwide,
unsafe drinking water is a major problem. However, international
travelers should not become hysterical about avoiding all
water whilst traveling abroad. Most of the general information
sites for travelers recommend to avoid drinking water anywhere
abroad. But to avoid water where it is safe, could be as annoying,
as dangerous to drink it where is not safe. Worldwide,
unsafe drinking water is a major problem. However, international
travelers should not become hysterical about avoiding all
water whilst traveling abroad. Most of the general information
sites for travelers recommend to avoid drinking water anywhere
abroad. But to avoid water where it is safe, could be as annoying,
as dangerous to drink it where is not safe.
Prevention of Travellers Diarrhoea
No vaccines
are available and none are expected to be available in the
near future that are effective against TD.
The
use of prophylactic antibiotics is not recommended for travellers
since there is little evidence to show that they are widely
effective in preventing TD and there are potential drawbacks
which include include allergic and other side effects and
the possibility of developing resistance.
Our
intestinal flora are thought to play an important role in
protecting us against infection and managing immunity. They
also provide specific enzymes needed to digest particular
substances in the diet.
Many digestive health problems including TD can escalate as
our fragile intestinal flora is disturbed by the environmental
and dietary changes associated with foreign travel.
Travellers
can minimise these digestive health risks by departing with
a well balanced and healthy intestinal flora and by maintaining
this protective shield throughout their travels.
Probiotics specifically developed for travellers are an effective
means to ensure a healthy and well balanced intestinal flora
by strengthening the healthy balance of friendly bacteria
in the gut and enhancing its protective capacity and by selectively
binding to harmful bacteria and flushing them out.
 However,
most evidence shows that meticulous attention to hygiene during
food and beverage consumption can greatly decrease the likelihood
of developing TD. However,
most evidence shows that meticulous attention to hygiene during
food and beverage consumption can greatly decrease the likelihood
of developing TD.
Many travellers, however, encounter difficulty in observing
these restrictions.
Some useful precautions include:-
- Unless
you are sure of the purity of the water supply, don't drink
it. This also applies to water used for ice-cubes and for
cleaning teeth.
- Water
from sealed lid bottles is usually safe, as are hot tea
and coffee, fizzy drinks, beer and wine.
- Take
care with local cheeses and ice cream. Boil unpasteurised
milk before use.
- Cook
meat thoroughly and eat while still hot. Avoid leftovers.
- Fish
and shellfish may be hazardous even if well cooked. Take
local advice, but avoid seafood if in doubt.
- Eat
only cooked vegetables and avoid salads.
- Peel
all fruit, including tomatoes. Avoid food exposed to flies.
- Wash
all dishes and cutlery in clean, hot water.
- Wash
your hands thoroughly before eating or handling food, and
always after using the toilet.
Treatment
of Travellers Diarrhoea
Travellers
with TD have two major complaints for which they desire relief;
abdominal cramps and diarrhoea.
 Oral
Rehydration Solution (ORS) Oral
Rehydration Solution (ORS)
Most
cases of diarrhoea are self-limiting and require only simple
replacement of fluids and salts lost in diarrhoeal stools.
This is best achieved by the use of oral rehydration solution
such as Dioralyte, Electolade, Rehidrat, or similar, which
is available in sachets of powder at stores or pharmacies
in almost all countries and must be prepared by adding the
contents of a sachet to boiled or treated water.
The
instructions should be checked carefully to ensure that the
powder is added to the correct volume of water. This solution
is appropriate for treating as well as preventing dehydration
and should be consumed or discarded within 12 hours if held
at room temperature or 24 hours if kept refrigerated.
| If
sachets of ORS are unavailable or you have run out, an
emergency alternative can be made up using eight teaspoons
of sugar and one teaspoon of salt added to one litre of
safe, drinkable water. |
Travellers
should be advised to avoid iced drinks and non-carbonated
bottled fluids made from water of uncertain quality. Milk
can aggravate diarrhoea in some people and travellers with
diarrhoea should avoid it.
 Antimotility
Agents Antimotility
Agents
Such
as loperamide and codeine come in convenient dosage forms
and provide prompt symptomatic but temporary relief of uncomplicated
TD by inhibiting intestinal movements.
They
slow down the motility of the gut and increase fluid absorption
by normalising the transit through the gut and restoring normal
stools. They also diminish diarrhoea and shorten its duration
thereby reducing fluid loss at the same time.
Antimotility
agents relieve discomfort and social disruption and are safe
and effective for otherwise healthy adults. They are best
used when sanitary arrangements are difficult such as a long
journey.
Self
medication with antimotility agents is appropriate following
sudden onset of increased bowel action with loose watery stools
in persons over 12 and under 75 years of age who were previously
in good health and not suffering from any other serious illness.
However,
they should not be used by people with high fever, with blood
in the stools, or if there is vomiting and dehydration. They
should be discontinued if symptoms persist beyond 48 hours
or they could make the illness worse.
 Antibiotic
Treatment Antibiotic
Treatment
travellers
who develop severe and prolonged diarrhoea especially if associated
with nausea, vomiting, abdominal cramps, fever, or blood in
the stools, would benefit greatly from antibiotic treatment.
Nausea and vomiting without diarrhoea should not be treated
with antibiotics.
The
most likely antibiotic regimen to be effective against enteric
bacterial infection is ciprofloxacin (500mg taken twice a
day), whilst metronidazole (800mg taken three times a day)
is usually effective against protozoan infection. There is
no antibiotic treatment effective against viral infection.
The
biggest problem facing the sufferer is being able to accurately
diagnose the cause which is virtually impossible without medical
training. Since the symptoms of bacterial infections develop
much more rapidly than protozoan infections it is safe to
assume that a sudden onset is a bacterial infection.
Medical assistance (if available) should always be
sought if any of the following occur:-
- There
is blood in the faeces
- There
is a fever
- The
sufferer becomes confused
- The
diarrhoea does not settle within 72 hours
However,
medical assistance is not always available and the sufferer
must decide whether or not to be treated using available antibiotics.
|
|
|
|
| |
|
 |
| SAA
Club 349 |
|
|
Copyright © 2002 -
Llantrisant Sub-Aqua Club. All rights reserved.
|
|

 Since the number of divers
travelling abroad in search of new and exotic locations in
which to dive is on the increase, there is a growing need
for information about health protection in these foreign countries.
Since the number of divers
travelling abroad in search of new and exotic locations in
which to dive is on the increase, there is a growing need
for information about health protection in these foreign countries. However,
most (but not all) of the world's
exotic dive locations are located in and around the
tropics and are accessed via developing countries,
where there are endemic health
issues and the
standard of healthcare is often below that of the UK.
However,
most (but not all) of the world's
exotic dive locations are located in and around the
tropics and are accessed via developing countries,
where there are endemic health
issues and the
standard of healthcare is often below that of the UK. The table below
contains information about vaccination requirements and malaria
prophylaxis for travellers going abroad and contains most
of the countries likely to be visited by divers going on diving
holidays and expeditions.
The table below
contains information about vaccination requirements and malaria
prophylaxis for travellers going abroad and contains most
of the countries likely to be visited by divers going on diving
holidays and expeditions. In addition to malaria
tablets and the various vaccinations required, persons travelling
to developing countries are strongly advised to carry a medical
kit containing a number of medical and first aid item.
In addition to malaria
tablets and the various vaccinations required, persons travelling
to developing countries are strongly advised to carry a medical
kit containing a number of medical and first aid item.
 The
list of countries in the table below is by no means exhaustive
and should only be used for quick reference purposes. The
data in the table only applies to healthy adults. Travellers
will need to consult their own doctor to arrange to have the
relevant vaccinations.
The
list of countries in the table below is by no means exhaustive
and should only be used for quick reference purposes. The
data in the table only applies to healthy adults. Travellers
will need to consult their own doctor to arrange to have the
relevant vaccinations.
 A: be Aware of the risk of malaria if you
are travelling to a foreign country.
A: be Aware of the risk of malaria if you
are travelling to a foreign country.  B: avoid mosquito Bites by taking appropriate measures.
Reducing the number of Bites reduces the chances of
getting malaria.
B: avoid mosquito Bites by taking appropriate measures.
Reducing the number of Bites reduces the chances of
getting malaria.  D: early Diagnosis of malaria if symptoms
manifest following travel to a malarious region is
vital. Malaria can be fatal but early diagnosis and
treatment is usually 100% effective.
D: early Diagnosis of malaria if symptoms
manifest following travel to a malarious region is
vital. Malaria can be fatal but early diagnosis and
treatment is usually 100% effective. Malaria is a disease
which you can catch by being bitten by a mosquito carrying
the malaria parasites in its saliva. The
species of mosquito that carries the malaria parasites is
the Anopheles mosquito.
Malaria is a disease
which you can catch by being bitten by a mosquito carrying
the malaria parasites in its saliva. The
species of mosquito that carries the malaria parasites is
the Anopheles mosquito.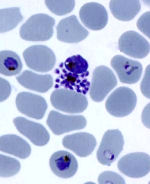 The
free parasites are then able to infect any mosquito that
feeds on your blood during this phase. The cycle then continues
as the parasites multiply inside the mosquito and invade its
salivary glands.
The
free parasites are then able to infect any mosquito that
feeds on your blood during this phase. The cycle then continues
as the parasites multiply inside the mosquito and invade its
salivary glands. Travellers'
diarrhoea (TD) is a condition characterised by a marked increase
in the frequency of unformed bowel movements and is commonly
accompanied by abdominal cramps, urgency, nausea, bloating,
vomiting, fever, and malaise.
Travellers'
diarrhoea (TD) is a condition characterised by a marked increase
in the frequency of unformed bowel movements and is commonly
accompanied by abdominal cramps, urgency, nausea, bloating,
vomiting, fever, and malaise. TD
is slightly more common in young adults than in older people
but attack rates are similar in men and women. It is possible
for travellers to experience more than one episode of TD during
a single trip but rarely is it life threatening.
TD
is slightly more common in young adults than in older people
but attack rates are similar in men and women. It is possible
for travellers to experience more than one episode of TD during
a single trip but rarely is it life threatening. Worldwide,
unsafe drinking water is a major problem. However, international
travelers should not become hysterical about avoiding all
water whilst traveling abroad. Most of the general information
sites for travelers recommend to avoid drinking water anywhere
abroad. But to avoid water where it is safe, could be as annoying,
as dangerous to drink it where is not safe.
Worldwide,
unsafe drinking water is a major problem. However, international
travelers should not become hysterical about avoiding all
water whilst traveling abroad. Most of the general information
sites for travelers recommend to avoid drinking water anywhere
abroad. But to avoid water where it is safe, could be as annoying,
as dangerous to drink it where is not safe.
 However,
most evidence shows that meticulous attention to hygiene during
food and beverage consumption can greatly decrease the likelihood
of developing TD.
However,
most evidence shows that meticulous attention to hygiene during
food and beverage consumption can greatly decrease the likelihood
of developing TD. Oral
Rehydration Solution (ORS)
Oral
Rehydration Solution (ORS) Antimotility
Agents
Antimotility
Agents Antibiotic
Treatment
Antibiotic
Treatment






